The pain of burn treatment
Pain is prevalent among burn survivors, with up to 48% reporting ongoing discomfort from their injuries.1 Dressing changes cause a reported 74% of patients to experience moderate to severe pain.2 This pain is more than simply discomfort; it can actively impede the healing process. Elevated pain levels can lead to increased stress responses, which may slow wound healing, and contribute to the development of chronic pain. With delayed wound healing there is also an increase in the risk of scarring. Therefore, addressing pain management affects patient outcomes burn care and healing.
The role of dressing selection in burn care pain management
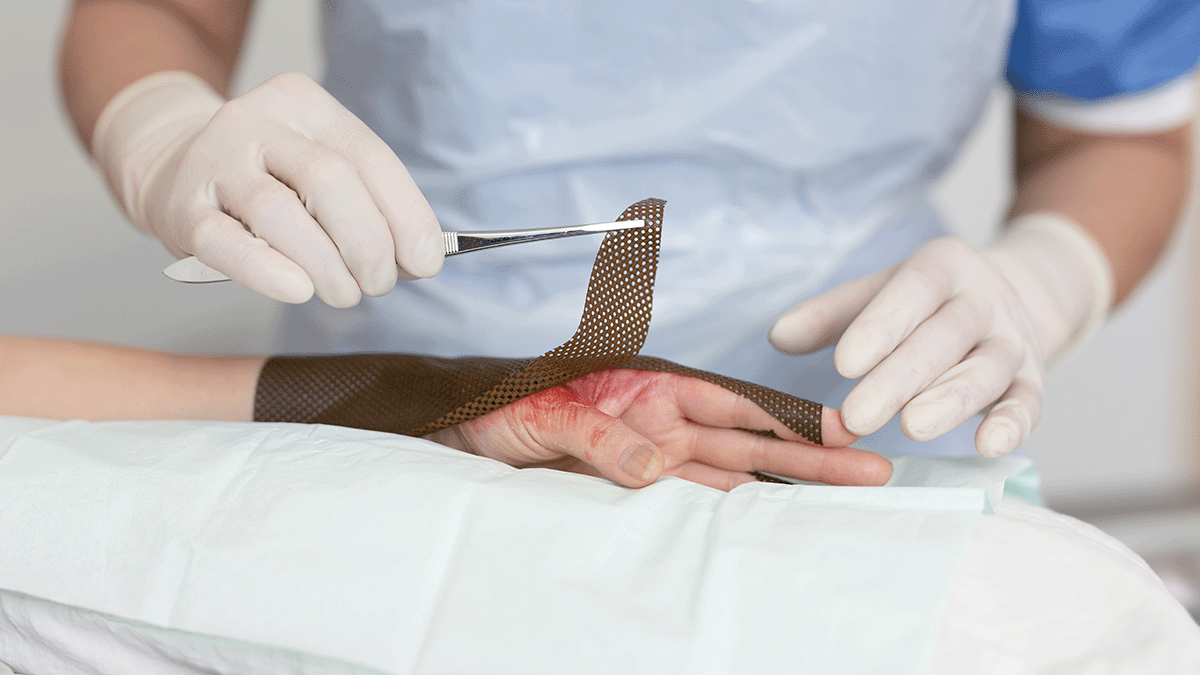
The choice of dressing determines a great deal in terms of whether it contributes to exacerbating or alleviating pain during treatment. Gauze in combination with silver sulfadiazine (SSD) cream or bacitracin often requires frequent changes. These frequent interventions can disrupt the wound environment, potentially leading to increased pain and delayed healing. Moreover, some traditional dressings may adhere to the wound bed, causing significant discomfort upon removal.
In contrast, modern silver-containing dressings have been developed to address these issues. These advanced dressings are designed to reduce adherence to the wound bed, minimising pain during dressing changes. Additionally, they often allow for longer intervals between changes, supporting undisturbed healing and reducing the frequency of painful interventions.
Benefits of silver-containing dressings over SSD cream
Silver sulfadiazine has been a standard topical antimicrobial agent in burn care for decades. However, recent studies have highlighted limitations associated with its use. For instance, SSD cream requires daily application and dressing changes, which can be painful and labour-intensive, particularly when frequent dressing changes disrupt undisturbed wound healing. Furthermore, some research suggests that SSD may delay wound healing and increase the risk of infection compared to modern alternatives.
Silver-containing dressings offer several advantages over SSD cream. These dressings provide sustained antimicrobial activity, maintaining a moist wound environment conducive to healing. They also require less frequent changes—often every few days instead of daily—thereby reducing the patient's exposure to contaminants and painful procedures. A comparative study found that silver-containing dressings are superior to SSD cream in managing superficial partial-thickness burns, leading to faster healing times, fewer dressing changes, and reduced pain during changes.3
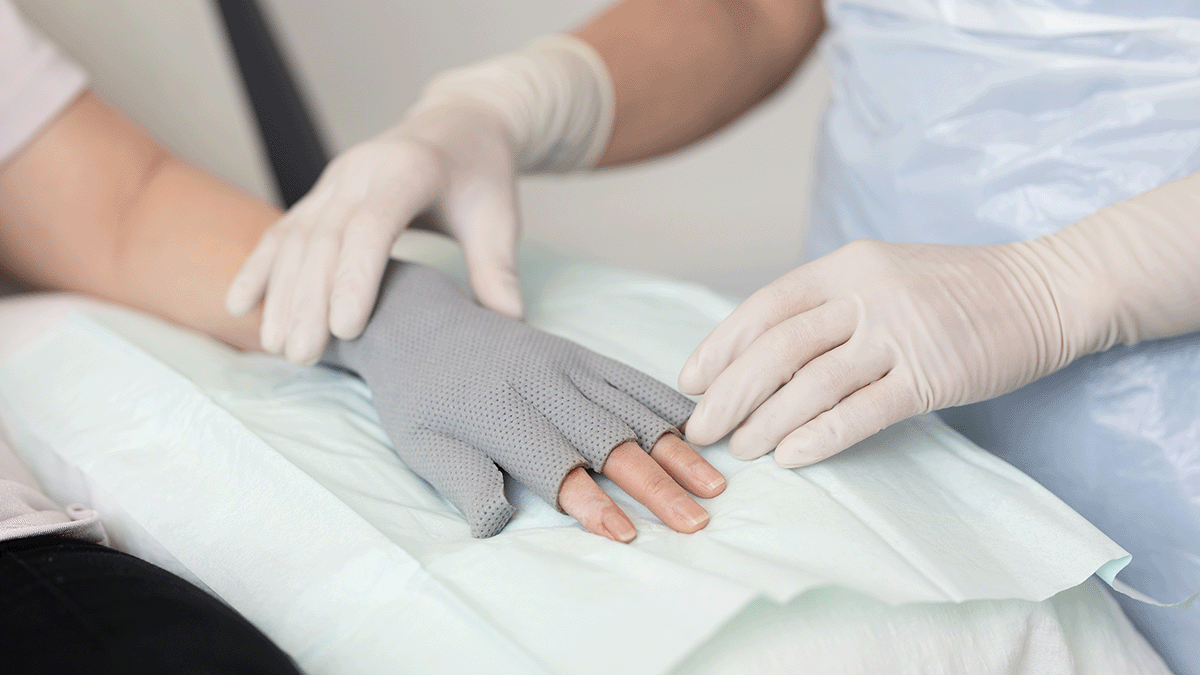
In addition, advanced dressings, such as Mepilex Ag, which feature a silicone wound contact layer, offer additional pain reduction. A silicone contact layer adheres gently to the skin without sticking to the wound and can be easily removed without damaging the skin.
Characteristics of an ideal burn dressing
The six key characteristics of an ideal burn dressing, ranked by importance, according to a global survey of burn care experts4 are:
- Anti-infectiveness
- Pain-free dressing change
- Pain reduction
- Lack of adhesion to wound bed
- High absorbency
- Requirement for fewer dressing changes
Modern silver-containing dressings with a silicone contact layer align well with these criteria, offering non-adherent surfaces, sustained antimicrobial activity, and the capacity for extended wear. By incorporating these dressings into burn care protocols, healthcare providers can enhance patient comfort, reduce the trauma associated with treatment, and promote more efficient healing.
Cost-effectiveness of modern dressings
While the initial cost of advanced silver-containing dressings may be higher than traditional options, they can be more cost-effective in the long run. The reduction in dressing change frequency decreases the labour and resources required for wound management. But the cost of the dressing is only one consideration. By minimising pain and trauma, these dressings can reduce the need for pain medication, potentially shorten hospital stays, and increase patient compliance. Atraumatic dressings also lower the risk of complications, which can lead to further cost savings.
Taking away the pain and trauma from burn treatment
Advancements in burn care have shifted the focus toward treatments that not only promote healing but also minimise pain and trauma for patients. Transitioning from traditional SSD cream to modern silver-containing dressings can also offer additional benefits, including fewer required dressing changes, and improved healing outcomes. By adopting these advanced dressings, healthcare providers can enhance the quality of care for burn survivors, facilitating a less traumatic, less painful journey to healing.