Providing cost-effective burn care is a multifaceted challenge that requires a comprehensive evaluation of various treatment modalities, particularly the selection of appropriate dressings. The choice of dressing not only influences the healing trajectory and can influence the overall cost of care. A thorough understanding of the cost-effectiveness of different burn dressings is essential for optimising patient outcomes while sustaining cost-effective care.
Understanding burn wound management
Serious burn wounds require complex and long-term management, potentially involving long hospital stays, time-intensive surgical and non-surgical treatments, pain management and rehabilitation. All of these have associated costs that result in burn care being expensive1.
The mean cost of burn care in a burn centre is more than three times higher than the mean cost of burn care in a general hospital.
The complexity and multidisciplinary nature of burn wounds make them particularly challenging, as they require comprehensive management to prevent complications, such as infections, delayed healing, and excessive scarring.
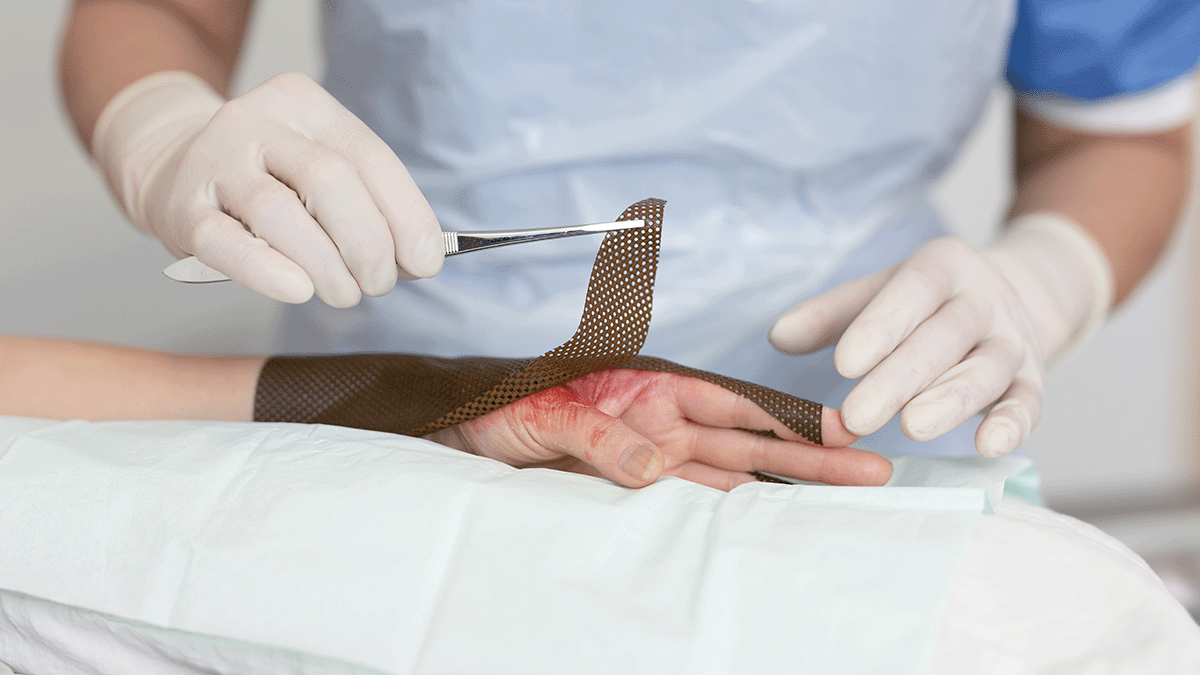
Burn dressings are one key element of this management, helping to provide a moist wound environment, protecting the wound from external contaminants, and delivering antimicrobial agents when necessary. But not all burn dressings are created equally. How can the cost-effectiveness of a burn dressing be measured?
Evaluating the cost-effectiveness of burn dressings
The cost-effectiveness of burn dressings is determined by analysing both direct and indirect costs associated with their use. Direct costs address the price of the consumable products used at each dressing change. Indirect costs include factors, such as associated labour cost, the length of hospital stay, incidence of infection, the need for additional treatments or surgeries, and overall impact on the patient’s quality of life.
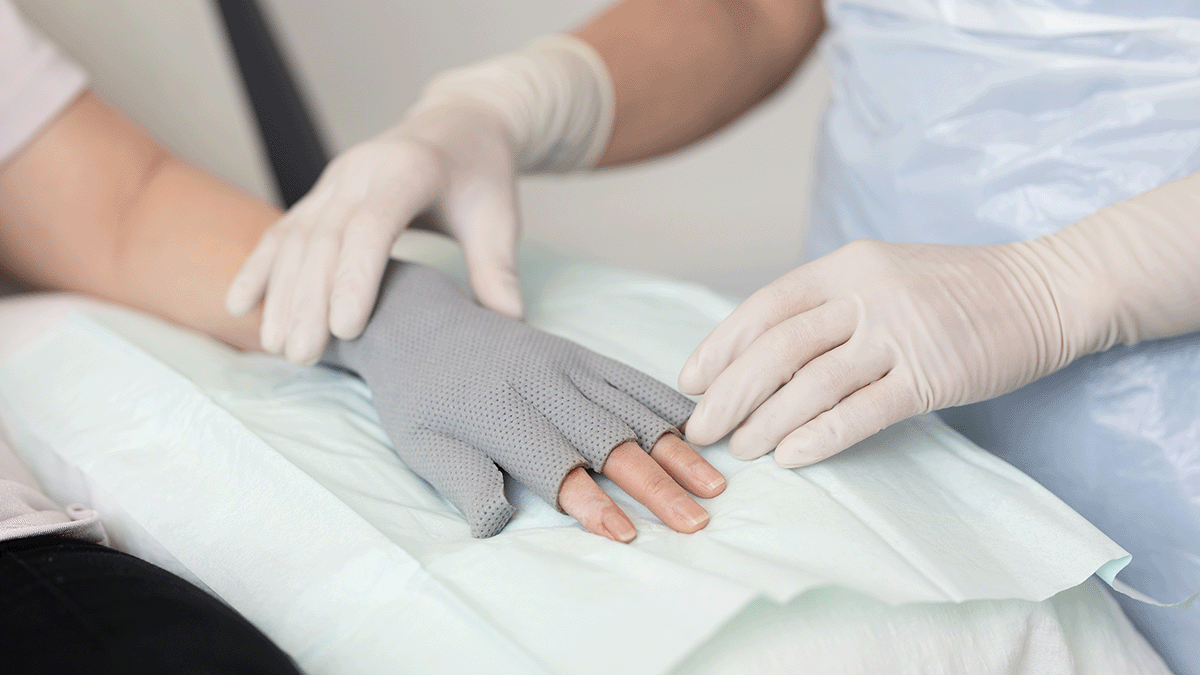
A study published in the Journal of Burn Care & Research compared the cost-effectiveness of a silver-containing soft silicone foam dressing to silver sulfadiazine cream in patients with partial-thickness burns2. The randomised, multicenter trial found that the silicone foam dressing was more cost-effective, primarily due to reduced frequency of dressing changes and lower associated labour costs. Patients treated with the silicone foam dressing also experienced less pain and greater comfort, contributing to improved patient satisfaction and potentially faster healing times.
Another prospective, randomised controlled trial3 evaluated four commonly used burn dressings in an outpatient setting. The study assessed factors, such as healing time, pain during dressing changes, and overall cost of treatment. The findings highlighted significant differences in performance and cost among the dressings, underscoring the importance of selecting dressings based on individual patient needs and specific wound characteristics to optimise both clinical outcomes and cost-efficiency.
Total cost of care considerations
When determining the most cost-effective dressing, it is important to adopt a holistic perspective that considers the total cost of care. This approach involves evaluating not only the unit cost of the dressing but also the broader economic implications of its use. For instance, a dressing that is more expensive per unit may prove to be more cost-effective in the long run if it leads to faster healing, fewer complications, and reduced need for additional interventions or hospitalisations. That is, some advanced dressings may have higher upfront costs, but their effectiveness in promoting healing and preventing complications can result in overall cost savings.
Balancing cost and clinical outcomes
Balancing cost considerations with clinical outcomes and efficacy is an increasingly common challenge in healthcare. Rising demand weighed against financial and resource constraints make cost containment a watchword throughout the healthcare sector. While cost is a critical factor, cost containment cannot be the sole consideration if short-term costs remove focus from long-term patient outcomes. From a procurement perspective, less expensive dressings selected solely as a cost-cutting measure can lead to higher costs in the long run, which runs contrary to the principles of value-based healthcare.
Value-based healthcare (VBH) aims to achieve the best possible outcomes with existing resources, which requires looking at the big picture. With regard to dressings, a holistic approach to understanding dressing properties demands calculating for factors beyond just price. That is, what is the total cost of healing a wound? Other factors to consider in making such a calculation include characteristics, such as dressing wear time, which affects the frequency of dressing change. Fewer dressing changes reduces the number of dressings required and the time nurses spend changing dressings.
Because the least expensive dressing is not necessarily the one that adds the most value, decisions regarding dressing selection should be individualised. In the case of burn dressings, taking into account the specific characteristics of the burn wound, patient preferences, and the clinical setting are important in balancing cost and clinical outcomes.
Comprehensive burn care demands total cost of care considerations
Providing cost-effective burn care is about more than surface-level, cost-per-unit calculations. Comprehensive burn care demands comprehensive evaluation of the total cost of care associated with different dressing options.
By considering both direct and indirect costs, as well as the clinical effectiveness of each dressing, healthcare providers can make informed decisions that optimise patient outcomes while ensuring cost-effective solutions.