Surgical incision wounds, often perceived as routine and straightforward aspects of postoperative recovery, have often been overlooked and underemphasised in wound care management. This oversight can lead to suboptimal healing outcomes and increased patient suffering as well as higher costs of care. Recent insights underscore the necessity of re-evaluating incision care and the pivotal role of dressing selection in promoting effective healing.
Surgical incisions: The forgotten wound?
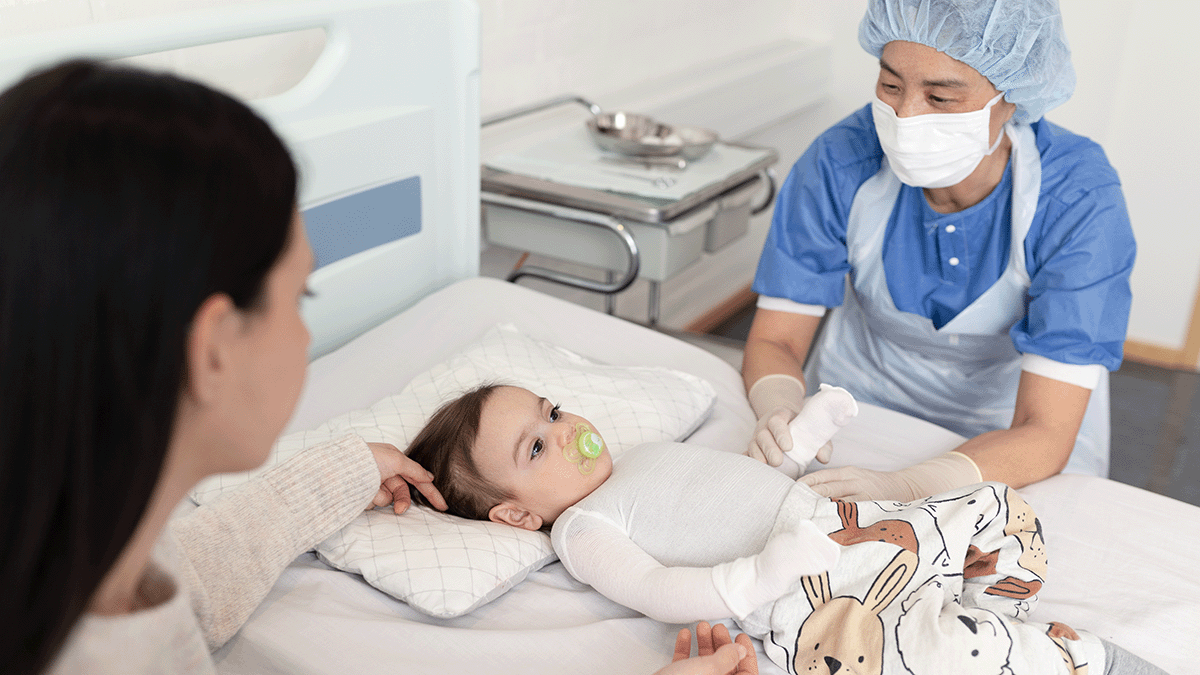
Within wound care, chronic wounds take most of the focus; they are complex and have prolonged healing processes. As a result, surgical incision wounds, which are acute by definition, may not receive as much attention from a clinical perspective. This disparity arises from the assumption that surgical wounds, being clean and surgically controlled, will heal without as much care or intervention. However, ignoring careful incision care also poses risks, such as complications like surgical site infections (SSIs) and wound dehiscence.
Rethinking surgical incision care
Rethinking surgical incision care advocates for a paradigm shift in how surgical incision wounds are managed. Central to this shift is the concept of undisturbed wound healing (UWH), which emphasises minimising interference with the wound site to foster optimal healing conditions. This approach involves selecting appropriate dressings that can remain in place for extended periods, thereby reducing the frequency of dressing changes and the associated risks of wound exposure and contamination.
Supporting undisturbed healing is the need to create and maintain a moist environment for optimal wound healing, both in acute and chronic wounds. Adopting undisturbed wound healing as a concept means allowing the healing process to progress uninterrupted, not disturbing the wound unless absolutely and clinically necessary2, 3. It is based on maintaining a constant temperature, an optimal moist environment and keeping the wound free of external agents to facilitate the normal wound healing process.
How, though, with traditional wound care protocols and conventional dressings, can healthcare providers reach an ideal undisturbed wound healing state?
The critical role of dressing selection in promoting UWH
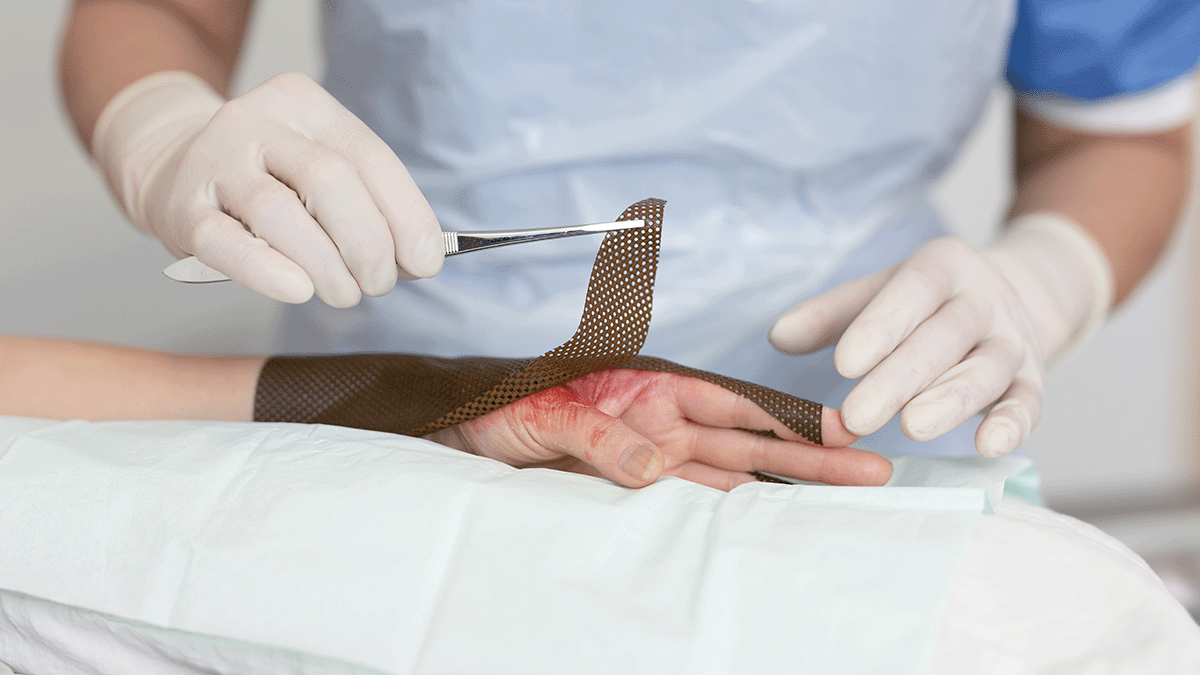
Post-op incision care immediately after surgical procedure is critical. Consensus in the literature2 indicate that dressings applied in the operating theatre should remain in place for as long as possible, changed when it is clinically needed rather than based on habits or protocols.
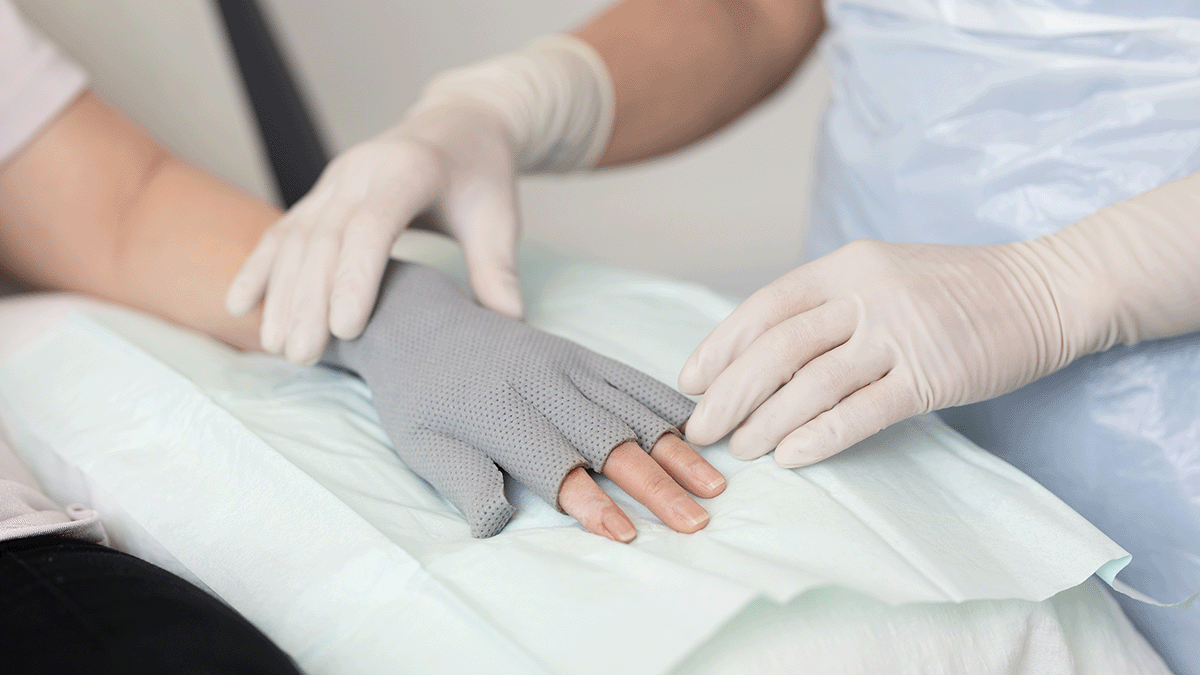
Being able to leave a post-op dressing in place for as long as possible means that dressing selection becomes critical. The ideal dressing should maintain a moist wound environment, provide thermal insulation, protect against bacterial contamination, and manage exudate effectively. Simple gauze is insufficient because it requires frequent changes and does not have the capacity or long-wearing properties of advanced dressings.
Advanced wound dressings have been shown to support the needed functions, thereby facilitating UWH. By keeping the wound environment stable and protected, these dressings can reduce the risk of SSIs and promote more efficient healing. Such dressings can stay in place for longer wear as recommended, using gentle adhesives that avoid blistering and peri-wound injuries. They are designed for good exudate management and absorption, and allow patients to shower and have a free range of motion4.
Clinical evidence supporting advanced dressing use
Clinical studies have demonstrated the benefits of advanced dressings in surgical wound management. For instance, a consensus document by the World Union of Wound Healing Societies (WUWHS) highlights that advanced dressings play a vital role in protecting wounds from surgical complications during the healing process. These dressings not only provide a barrier against external contaminants but also create an optimal environment for cellular activities essential for wound repair.
Economic considerations and patient outcomes
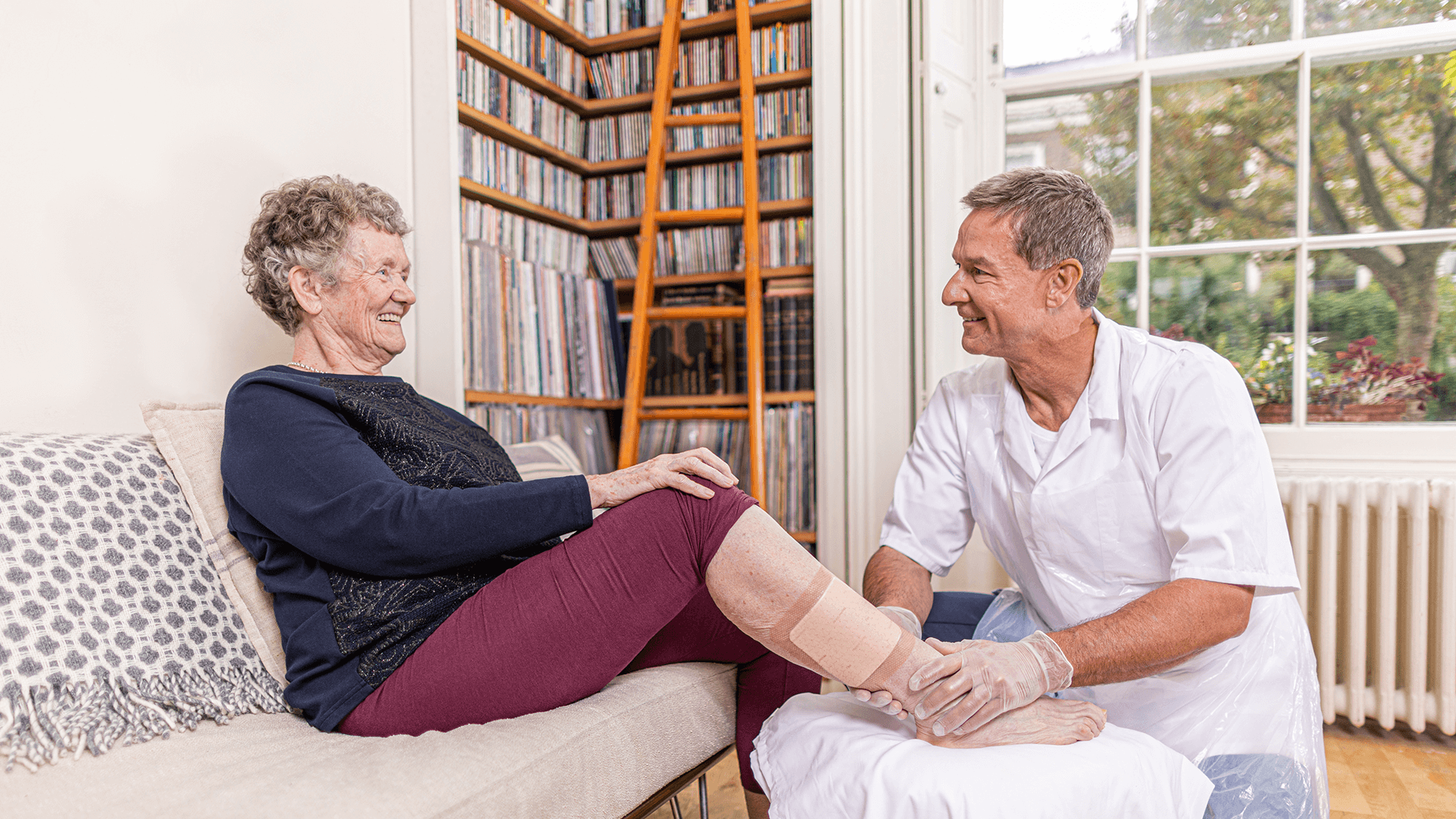
While advanced dressings may incur higher initial costs compared to traditional gauze, the overall economic impact works out to be a lower cost of care when considering the bigger picture. The use of advanced dressings can lead to fewer dressing changes, reduced labour costs for healthcare providers, and a decrease in the incidence of complications that require additional treatments. Moreover, improved patient outcomes, such as faster healing times and reduced discomfort, contribute to enhanced patient satisfaction and quality of life.
Implementing best practices in incision care
Optimising surgical incision care will require rethinking incision care, dressing protocols and dressing selection. Healthcare providers are on the frontlines and should consider the following best practices:
- Assessment of wound characteristics: Evaluate the wound's size, location, exudate level, and patient-specific factors to inform dressing selection.
- Selection of appropriate dressing: Choose dressings that support UWH by maintaining a moist environment, managing exudate, and providing a barrier to contaminants.
- Minimise dressing changes: Limit dressing changes to when clinically indicated, such as signs of infection or dressing saturation, to reduce disruption of the wound environment.
- Patient education: Inform patients about the importance of UWH, signs of potential complications, and the need to avoid unnecessary removal and change of the dressing.
- Monitoring and documentation: Regularly assess the wound and document its progress to ensure timely identification of any issues and to adjust care plans accordingly.
Making incision care matter
Surgical incision wounds should no longer be the forgotten aspect of wound care. By rethinking incision care and prioritising the selection of advanced dressings that facilitate undisturbed wound healing, healthcare providers can improve patient outcomes, reduce complications, and achieve more efficient use of healthcare resources.