Diagnosis, treatment and management of DFUs
Successful diagnosis and treatment of diabetic foot ulcers involves a holistic approach that includes the patient’s physical, psychological, and social health and the status of the wound1.
The management of diabetic foot ulcer begins with assessment, grading, and classifying the ulcer based on clinical evaluation of the extent and depth of the ulcer and the presence of infection, which determines the nature and intensity of treatment2 3 . The degree of ischaemia for patients with diabetic foot ulcers is assessed by ankle-brachial index (ABI) and toe pressure measurements3 . To test the peripheral neuropathy there are two simple and effective tests used:
- 10 g Monofilament for testing the sensory neuropathy should be applied at various sites along the plantar aspect of the foot.
- Tuning fork standard 128Hz is used to test the ability to feel vibrations; a biothesiometer is a device that also assesses the perception of vibration1
In patients with peripheral neuropathy, it is important to offload at-risk areas of the foot in order to redistribute pressures evenly4. Inadequate offloading leads to tissue damage and ulceration.
To ensure holistic assessment and treatment of diabetic foot ulcers, the wound should be classified according to a validated clinical tool. The University of Texas (UT) system was the first diabetic foot ulcer classification to be validated and consists of three grades of ulcer and four .
Holistic patient assessment and M.O.I.S.T. framework
The management of hard-to-heal wounds relies on performing a holistic assessment of the person with a wound, using a framework that helps deliver optimal wound treatment.
M.O.I.S.T. is such a framework, which encourages a systematic approach. It provides healthcare professionals guidance for planning and education with regard to local therapy6. The acronym M.O.I.S.T. represents:
- Moisture Balance
- Oxygen Balance
- Infection Control
- Support
- Tissue
Learn more about M.O.I.S.T. at Clinical Learning Hub or take a more playful approach to learning about M.O.I.S.T. in Microworld.
Debridement and inspection
The European Wound Management Association (EWMA) states that the emphasis in wound care for diabetic foot ulcers should be on radical and repeated debridement, bacterial control and frequent inspection and careful moisture balance to prevent maceration7. The patient’s vascular status must always be determined prior to sharp debridement. Patients needing revascularisation should not undergo extensive sharp debridement because of the risk of trauma to vascularly compromised tissues1.
While it may seem logical that effective glucose control could promote healing of diabetic foot ulcers, there is no evidence in the published literature to support this assumption8. An explanation for this finding may be that small vessel diabetic arteriolosclerosis is irreversible and after a certain time is not responsive to normoglycaemia8.
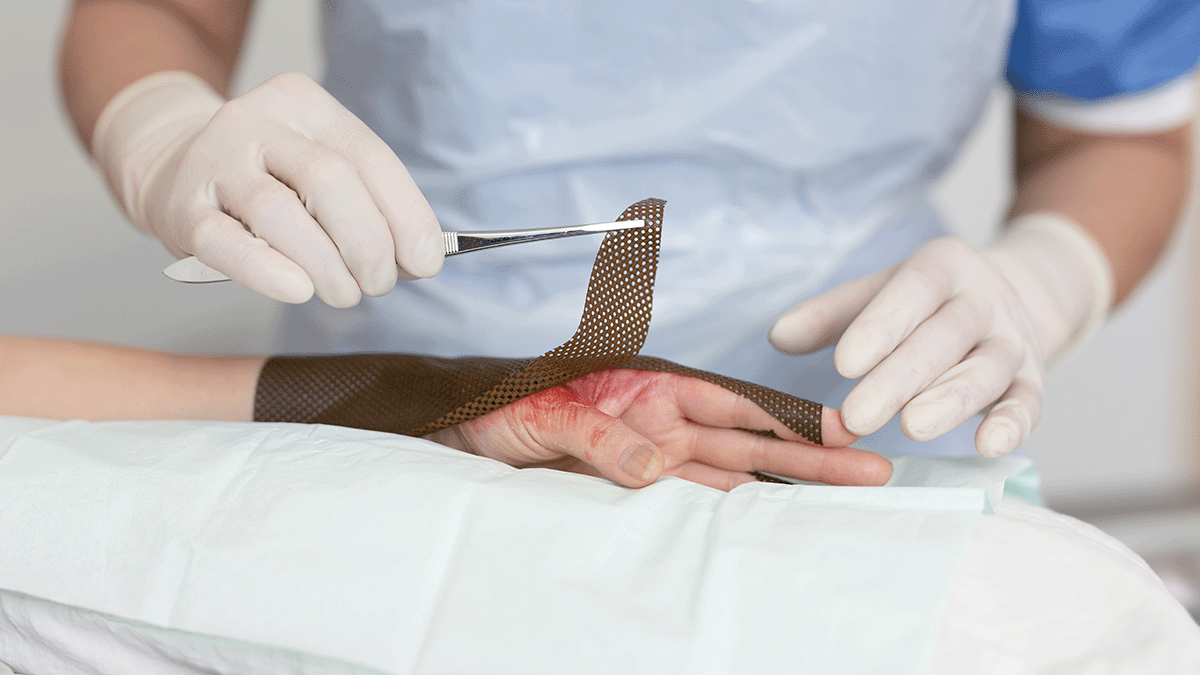
The role of dressings in the management of diabetic foot ulcers
Following debridement, the diabetic foot ulcer should be kept clean and moist but free of excess exudate, with wound dressings selected based on the ulcer’s characteristics, such as the extent of exudate or necrotic tissue9. Some dressings are also impregnated with antimicrobial agents to prevent infection and enhance ulcer healing10. Should infection occur, infection management is critical for promoting continued healing, including antibiotic treatment and the use of diagnostic tools like X-rays to rule out osteomyelitis.
By using a dressing that creates a moist wound healing environment, a natural process to soften and remove devitalised tissue will occur. This process is called autolytic debridement. Care must be taken not to use a moisture-donating dressing, as this can predispose the skin to maceration. In addition, the application of moisture-retentive dressings in the presence of ischaemia and/or dry gangrene is not recommended11 12.
It is important to incorporate strategies to prevent trauma and minimise wound-related pain during dressing changes13. This may include the use of soft silicone dressings and avoiding unnecessary manipulation of the wound14. It is now acknowledged that many patients, even those with neuropathy or neuroischaemia, can feel pain due to their wound or a procedure14.
Other advanced treatments for diabetic foot ulcers
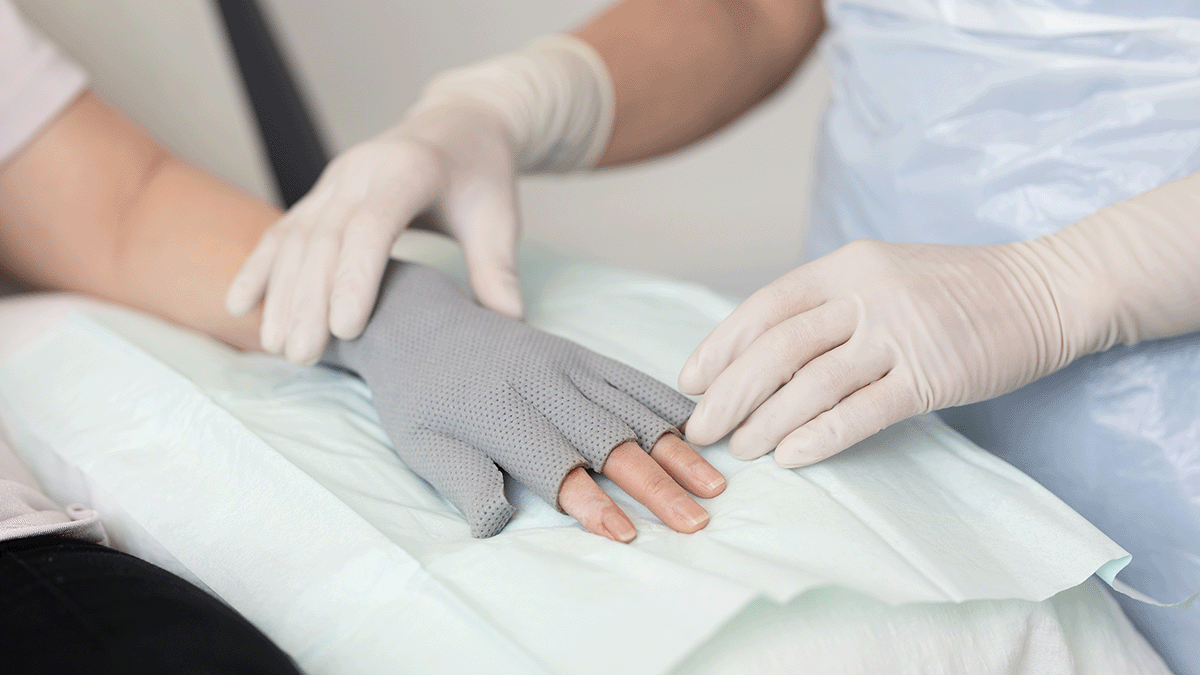
Adjunctive therapies may improve ulcer healing, such as negative pressure wound therapy (NPWT), the use of custom-fit semipermeable polymeric membrane dressings, cultured human dermal grafts, and application of growth factors15.
All ulcers subjected to sustained or frequent pressure and stress, including pressure-related heel ulcers or medial and lateral foot ulcers or repetitive moderate pressure (plantar foot ulcers) benefit from pressure reduction, which is accomplished with mechanical offloading. Offloading devices include total contact casts, cast walkers, shoe modifications, and other devices to assist in mobility15.
Patient education for foot and DFU self-care
Effective foot care should be a partnership between patients, carers and healthcare professionals. Educating patients about proper foot care and periodic foot examinations are effective interventions to prevent ulceration16.