Venous leg ulcer management guidelines and consensus recommendations
There are several guidelines and consensus recommendations for the management of VLU.1, 2 Some documents focus on compression therapy.3, 4 A comprehensive assessment of the patient, the wound, and the surrounding skin should be made on initial presentation and at frequent intervals to guide ongoing management.1, 2, 5
Wound bed preparation and wound assessment
The management of chronic or hard-to-heal wounds relies on the holistic assessment of the person with a wound, using a framework that can help deliver optimal wound treatment.
TIME is one of the methods used for wound bed preparation6, 7, 8, 9 comprising four components that underpin wound bed preparation:
- Tissue management
- Inflammation and infection control
- Moisture balance
- Epithelial (edge) advancement7
M.O.I.S.T. is another similar concept, which also encourages a systematic approach to wound assessment. The M.O.I.S.T. concept provides healthcare professionals with guidance for systematic planning and education with regard to local therapy.20
M.O.I.S.T. represents five principles that support wound management:20
- Moisture Balance
- Oxygen Balance
- Infection Control
- Support
- Tissue
Risk of infection
Chronic non-healing wounds of the lower extremities are susceptible to infection, which can lead to serious complications, such as delayed healing, cellulitis, enlargement of wound size, debilitating pain, and deeper wound infections causing systemic illness.10, 11
Compression therapy and wound debridement can encourage clearing of the infection and help to promote healing.11 Antimicrobial dressings may be used in the short term for the treatment of wound infection.8 There is no evidence to support the routine use of systemic antibiotics to promote healing in VLU.11, 12
Exudate management in venous leg ulcers
Patients with VLU generally have an increase in wound exudate when compared with patients with other forms of chronic skin ulcers.13 Poor management of wound exudate can have a negative effect on patient quality of life and is associated with damage to the wound bed and peri-wound region, increased risk of infection, delayed wound healing, and increased costs to health services.13
Appropriate dressing selection and use in combination with the appropriate and sustained compression therapy work in conjunction to reduce excessive exudate levels².
Compression therapy
Compression therapy is widely recognised as key to the management of VLU. Compression therapy increases healing rates in comparison with no compression therapy,14 and after healing, reduces recurrence rates.15
A variety of devices are used for compression therapy, including different types of bandages, bandage systems, and garments that provide sustained compression, and pneumatic devices can apply intermittent compression.12
It is essential that underlying aetiology is established, and arterial disease excluded before treating a lower leg ulcer with compression therapy. This can be done through a combination of holistic assessment and simple investigations. In 15-20% of VLU an arterial impairment coexists,16 and these ulcers are known as ‘mixed ulcers’. Arterial impairment is assessed by measuring the ratio between the ankle and the brachial pressure (ABPI), which is more than 0.95 in normal subjects.17 Compression therapy must be avoided in severe, critical limb ischaemia.12
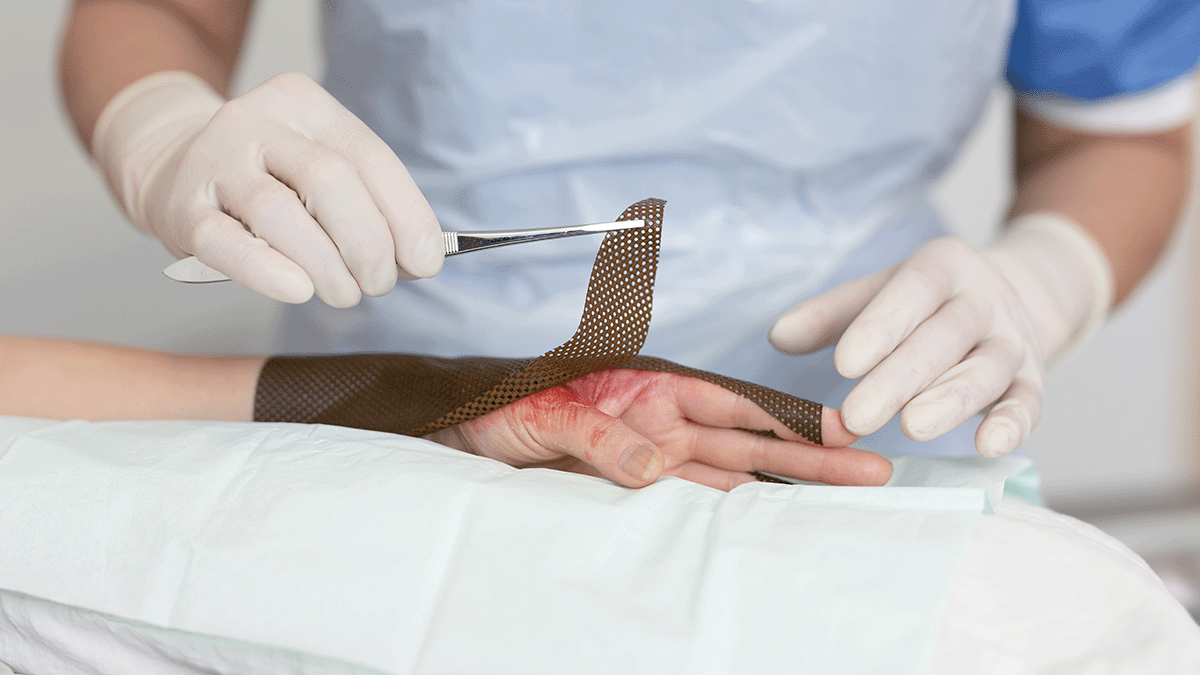
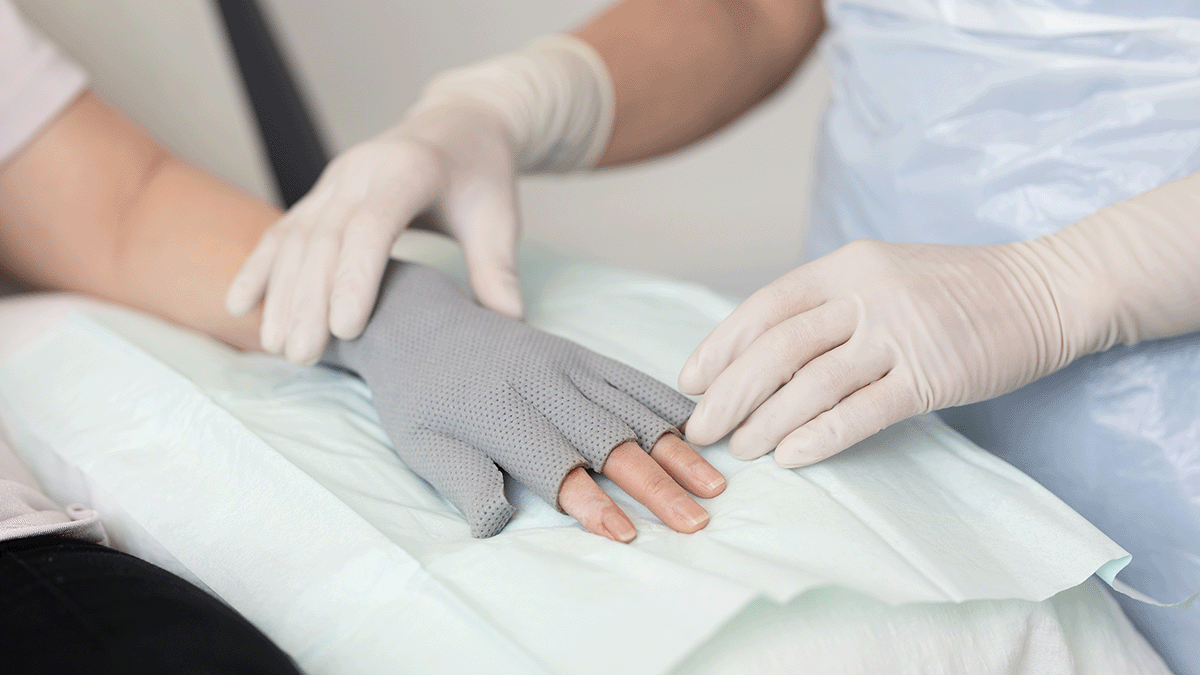
The role of dressings in the management of venous leg ulcers
Ulcers of the skin require wound dressings for protection from further trauma, prevention of progression, and treatment. Because VLU are associated with high levels of exudate that contain proteases and inflammatory cytokines that may damage surrounding healthy skin, current guidelines recommend the use of wound dressings that manage wound exudate while maintaining a moist wound bed.12, 18
The effective management of wound exudate has been shown to reduce time to ulcer healing, to reduce the risk of skin damage and infection, and to enhance patient quality of life and improve healthcare clinical and cost efficiency.
The dressing selected should be:
- effective under compression therapy, i.e., retain moisture without leaking when placed under pressure.
- atraumatic without damaging the wound bed or peri-wound skin on removal.
- comfortable and conformable to the wound bed.
- of low allergy potential.
- still intact on removal.
- low profile (unlikely to leave an impression in the skin).
- cost-effective, i.e., offer optimal wear time.2