No oxygen – no healing
Chronic wounds share a common challenge: a lack of oxygen reaching the wound. Wound healing requires large amounts of oxygen1, 2, 3 and healing is delayed when insufficient oxygen is available in the wound. A sustained failure of oxygenation at the tissue level – one of the barriers to healing for chronic wounds – is called hypoxia.1

Adapted from Hauser 1987*
Patients with chronic wounds, such as pressure ulcers, diabetic foot ulcers and venous leg ulcers, suffer from underlying conditions that compromise the body’s ability to move oxygen to the wound. The situation is worsened by a combination of reduced blood flow in the region of the wound, due to underlying diseases, such as diabetes or chronic venous insufficiency, and less efficient2, 3 healing because the wound healing process consumes more oxygen.1
*Hauser CJ. Tissue salvage by mapping of skin surface transcutaneous oxygen tension index. Archives of surgery (Chicago, Ill : 1960) 1987; 122(10): 1128-30.
Delivering oxygen for healing
Oxygen therapies can be delivered from the inside or outside (topically) of the body. Both approaches influence wound healing in different ways.1
Oxygen provided from the inside via hyperbaric treatment improves oxygen supply thanks to improved blood oxygenation, but this effect is temporary and best used as an adjunct treatment.1
Oxygen provided from the outside via various topical oxygen therapy methods facilitates the availability of oxygen to the base of the wound1. This can lead to sustained healing but needs a vehicle for diffusing oxygen and penetrating the wound’s exudate layer. Wounds are not able to access oxygen from the air – the atmosphere is 21% oxygen, but the diffusion rate of oxygen is reduced substantially when a thin liquid layer is present in the wound. Haemoglobin helps to transport oxygen to low-oxygen environments in the wound bed, naturally moving to where oxygen is most needed.
Topical haemoglobin treatment is a simple way to facilitate oxygen diffusion directly within a chronic wound.1 A haemoglobin spray can be applied to a wound as an adjunct to standard therapy1 to accelerate oxygen delivery4.
Controlling for condition-specific symptoms is central to healing – but this plays just one role in a host of therapies that contribute to successful healing of chronic wounds.
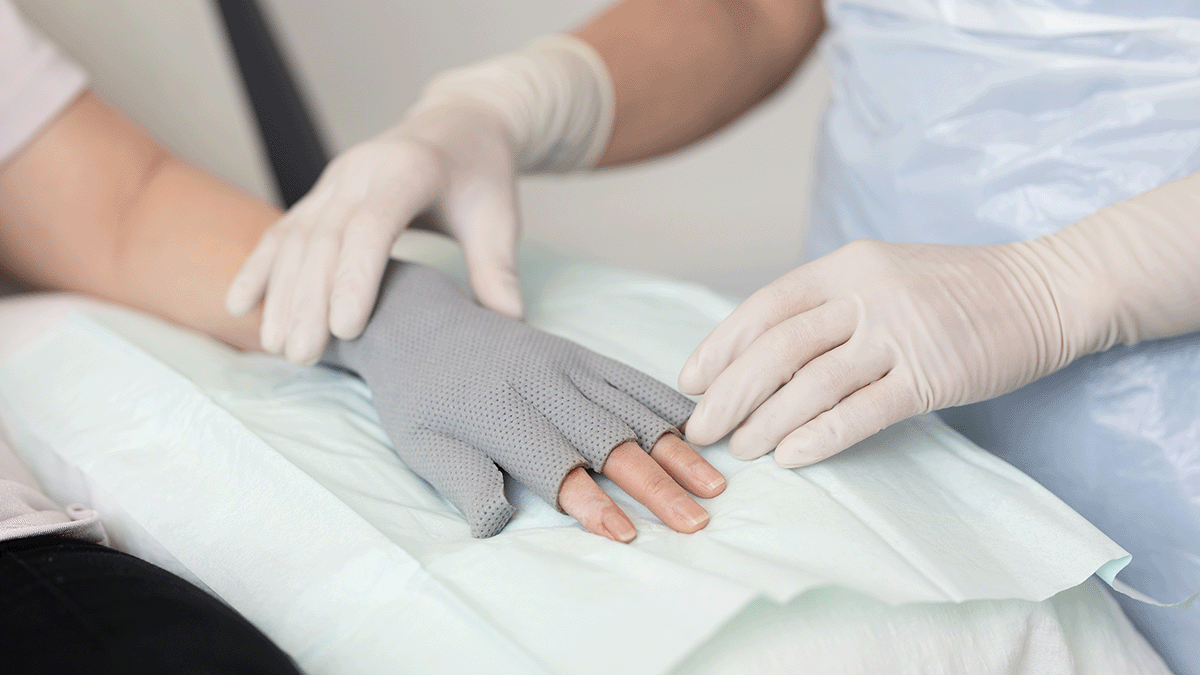
Helping oxygen reach the wound bed
Using a topical, purified haemoglobin spray on hard-to-heal wounds provides a direct channel for oxygen-loaded haemoglobin to diffuse through wound exudate5 and reach the wound for increased oxygen saturation.
In vivo measurements have demonstrated the increase in tissue oxygenation following topical application of haemoglobin spray (Granulox) on chronic wounds:
- Haemoglobin (Hb) spray (Granulox) is sprayed. Hb diffuses into the wound exudate and starts binding oxygen5
- Oxygen is readily available at the surface, and Hb binds more oxygen5
- Hb diffuses within the wound bed5
- Driven by the oxygen gradient, Hb releases oxygen to hypoxic regions6, contributing to multiple cycles of binding and release of oxygen
- The process is reversible, and Hb can absorb more oxygen where available
Granulox spray as topical oxygen therapy: Evidence-based oxygenation
Research supports the efficacy of wound oxygenation using facilitated diffusion. A EWMA group of experts has assessed the various treatment options available for addressing non-healing wounds1, citing topical oxygen therapy as offering accelerated healing with a high level of accessibility and ease of use, even for at-home use by patients.
Clinical studies report that using Granulox haemoglobin spray leads to shorter healing time, reduced pain scores and total cost savings for healthcare providers compared to the standard of care4.
- Twice as many chronic wounds healed at 8–16 weeks compared to standard of care6
- Time to heal diabetic foot ulcers was 50% shorter than with standard of care7
- More than 70% of patients reported lower average pain scores at four weeks than with standard of care in chronic wounds4
- 99% less slough in chronic wounds after four weeks compared to 33% with standard of care8
Proven oxygenation in minutes
Granulox delivers proven oxygenation to the wound bed in minutes. Imaging shows (see below), for example, a leg ulcer before Granulox treatment. Large areas are visible showing areas that are deoxygenated or receiving no oxygen at all. The second image shows the same wound 20 minutes after Granulox is applied, increasing oxygenation from 56% to 79% saturation.

3D imaging of a leg ulcer shows 56% O2 saturation, with large areas of deoxygenated Hb (blue) and no Hb (black)

79% saturation, 20 minutes after Granulox (p=0.043), with large areas of oxygenated Hb (red and white)
The patient perspective on topical oxygen therapy
For patients who have lived with chronic, hard-to-heal wounds, introducing a therapy that starts to show progress makes a difference to quality of life.
Granulox is safe, easy to use and cost-effective adjunctive therapy to standard wound care treatment.