Effective post-operative incision care is crucial for promoting optimal wound healing and minimising complications, such as surgical site infections (SSIs) and surgical wound dehiscence (SWD). A key component of this care is the selection of appropriate dressings that support long wear time and adopting a dressing change protocol that supports undisturbed healing (UWH). This article looks at findings from a series of international consensus meetings, highlighting best practices in incision care and dressing selection and care protocol to facilitate UWH.
Understanding undisturbed wound healing (UWH)
Undisturbed wound healing refers to the process by which a surgical incision heals without unnecessary interference or disturbance. Maintaining a stable wound environment is essential, as frequent dressing changes or external disruptions can impede the natural healing process, increase the risk of infection, and contribute to patient discomfort. The goal is to create conditions that allow the wound to progress through the normal stages of healing efficiently.
Promoting UWH and challenging ritualistic dressing changes
Traditional dressing change protocols rely on changing dressings on a schedule, whether or not a change is needed. This can unnecessarily disturb wound healing, potentially slowing or stopping healing entirely. Disturbing the wound exposes post-operative wounds to risk of contamination and increases the risk of a superficial surgical site infection (SSI). Post-operative dressing change protocols need to change to reflect changing clinical understanding.
At the same time, post-operative healing can benefit from rethinking postop dressing selection. Traditionally, post-operative wound care is dominated by conventional dressings, typically comprising a non-woven with an acrylic adhesive and an absorbing pad. These dressings tend to be low absorbing, lack barrier function and often cause painful skin damage. This type of dressing has been used for decades along with traditional protocols and ritualistic practice.
Charting a path toward undisturbed healing
Promoting UWH means challenging the 'it’s always been done this way' approach that prioritises frequent dressing changes necessitated by poor-absorption dressings. In the big picture, including total cost of care and patient comfort, the traditional way of postop dressing change can lead to the risk of contamination, higher costs of care in both material and clinician time, disturbed and delayed healing, and patient discomfort and pain.
But what should a post-operative dressing protocol look like? What should be demanded of a post-operative dressing?
Consensus recommendations on incision care
These kinds of questions were discussed by a team of senior surgeons who came together to ask how post-operative dressing challenges could be better handled. The conclusions were published as Incision care and dressing selection in surgical wounds: Findings from an international meeting of surgeons.
In addition to focusing on the importance of undisturbed wound healing, the international consensus group also highlighted the critical need to rethink postop dressing protocols for optimal healing.
The consensus meetings yielded valuable insights into best practices for incision care:
- Preoperative optimisation: Assess and optimise patient factors such as nutrition, glycemic control, and smoking cessation to enhance healing potential.
- Aseptic technique: Employ strict aseptic techniques during surgery to minimise contamination.
- Dressing application: Apply dressings in a manner that ensures full coverage of the incision without tension, preventing potential entry points for pathogens.
- Monitoring and assessment: Regularly assess the wound for signs of infection or other complications, but avoid unnecessary dressing changes if the dressing remains intact and exudate levels are manageable. The consensus found that dressings are changed too frequently and should only be changed when there is a clinically relevant reason to do so, such as saturated or leaking dressing, excessive bleeding, suspected infection, or potential dehiscence. Otherwise, leave the dressing in place – undisturbed.
- Patient education: Educate patients on signs of infection, proper wound care, and the importance of minimising disturbance to the wound site. Patients often have preconceived ideas of how often a dressing should be changed, i.e., too frequently, and will also benefit from learning the value of undisturbed healing. Clinicians should share the rationale and benefits of undisturbed healing with patients and be able to communicate these reasons effectively.
Regional considerations
While these general principles broadly apply, regional variations in healthcare practices, patient populations, and environmental factors mean that locally tailored approaches to incision care are needed. For instance, in regions with higher ambient temperatures, dressings with enhanced breathability may be preferred to prevent moisture accumulation. Cultural practices and patient preferences should also be considered to ensure adherence to care protocols.
Ideal post-op dressing protocol
The World Union of Healing Societies (WUWHS) recommends using a dressing that allows for a long wear time in order to promote undisturbed healing. Because existing dressing change protocols can depend so much on routine, ritual and habit, the goal is to change the mindset to move away from scheduled dressing changes toward promoting undisturbed healing with dressing changes based on clinical need.
In addition to moving away from ritualistic dressing change, the needs and preferences of patients are also important. This is important in post-op incision care, which has its own clinical needs. Consideration should be given to individual needs and preferences, the wound type and condition, and the appropriate dressing selection.
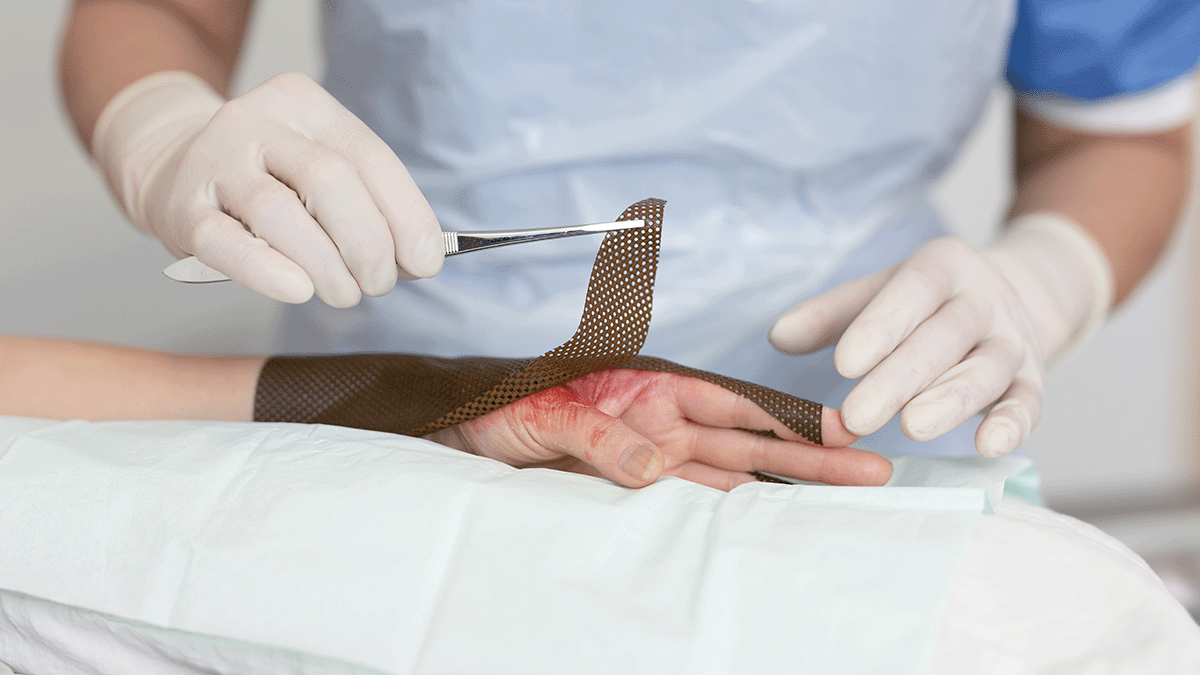
The role of dressing selection in UWH
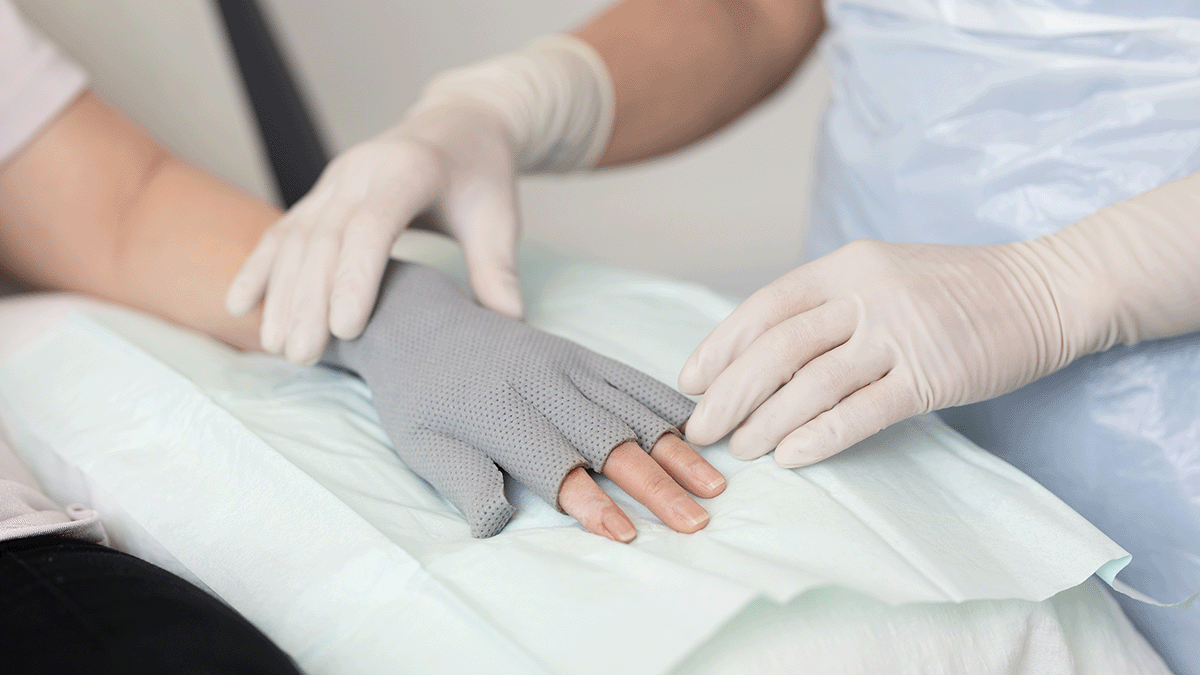
Selecting the appropriate dressing is central to supporting UWH. An ideal post-operative dressing should:
- Flexible (not impede the patient’s movement), providing elasticity to avoid pulling the skin or blistering (e.g. particularly over knee joints)
- Well fixed to the skin on application, even if the wound has been disinfected shortly before
- Absorbent, able to handle exudate
- Skin protective (e.g. reduce the risk of
blistering or irritation, not excessively
adhesive) - Waterproof: providing a good seal/barrier function and enabling the patient to shower
- Eliminate dead space between the dressing and the wound.
Advanced wound dressings have been designed for long-wearing protection and comfort, making them ideal post-op dressings.
Undisturbed healing: The goal of modern post-operative incision care
Undisturbed wound healing is a primary goal of modern post-operative incision care. By selecting appropriate dressings and adhering to best practices focused on undisurbed wound healing, healthcare providers can create an optimal incision healing environment, reduce the risk of complications, and improve patient outcomes. Ongoing education, patient engagement, and consideration of regional factors are essential components of effective incision management strategies.