Revolutionise care for people and planet
Transforming care for patients and caregivers
At Mölnlycke, we have always been dedicated to improving quality of life for patients and those who care for them. We do it by offering innovative, high-quality solutions for wound care and surgical procedures, and by helping you implement new, better ways of working. Ultimately, we enable safer, more efficient and more sustainable care. For people and planet.
-
Wound care solutions
Explore our offer of innovative solutions that are optimised for health care workflows while improving quality of care for patients.
Discover our wound care solutions -
Surgical solutions
A safe and stress-free care environment, where clinicians can perform at their very best, doing the job they care most about.
Discover our surgical solutions
We're here to help
If you have any question about our products and solutions or need assistans, contact our sales team. We look forward to helping you find the perfect solution for your needs.
Contact usLatest updates
Discover our latest offers and campaigns.
Let's make room for what matters
There are many examples of non-value added tasks, in or around the OR, that could easily be eliminated, simply by implementing more efficient ways of working.
Read more-
Find the right antiseptic product
Our antiseptic products are gentle on the skin and effective on microbes with long lasting effect. Support skin integrity and reduce the potential of infections.
Read more -
Introducing the new Mepilex Up:
An innovative foam dressing designed for exuding wounds.
Read more

‘I always double-glove, and have from the very beginning. It's never been a challenge to work this way.’
David Revez Neurosurgeon
Latest news
Read all news-

Mölnlycke Health Care publishes Annual report for 2024
“Our strong financial position and continued growth allow us to direct our future and continued investments. At the same time, it is clear that our strategy and previous investments have paid off, enabling close relationships with our customers working alongside them to handle the challenges of healthcare today,” says Zlatko Rihter, CEO of Mölnlycke. Highlights from the year: Continued strong growth at 7.4% compared to previous year and annual sales of EUR 2,064 million with improved profitability. The progress in becoming a leader in sustainable healthcare was recognised with a platinum medal from EcoVadis. Focus on transformation through partnerships commenced in 2024 with the acquisition of P.G.F. Industry Solutions, the strategic partnership with Ondine Biomedical Inc and strategic investments in MediWound and Siren. The joint venture Tamer Mölnlycke Care in Saudi Arabia has started production and there are plans for expansion in India and China. Download and read the full report on www.molnlycke.com/corporate/about/reports For more information, please contact: [Contact card] Sofia Lindqvist
-

New study demonstrates the potential benefits of dressing regime improvements in delivering value-based chronic wound care
Barcelona, Spain. 27 March 2025. New study reports that switching patients with chronic wounds to the multi-layered, bordered silicone-coated foam dressing, Mepilex® Border Flex, alongside a clinician educational support programme, resulted in a significant reduction in the number of dressing changes being undertaken and a reduction in dressing-related costs.1 The study, sponsored by Mölnlycke Health Care, and conducted across primary care facilities in Seville, Spain was today presented as an e-poster at the 35th Conference of the European Wound Management Association (EWMA) 2025 in Barcelona, Spain by the principal investigator Dr Andres Roldan Valenzuela, Centro de Salud Mairena del Aljarafe – Cuidad Expo, Seville. The primary outcome of the study was a statistically significant reduction in the number of dressing changes undertaken, prior to and after the switch from a bordered foam dressing (baseline) to Mepilex® Border Flex; results demonstrated the median number of dressing changes reduced during the study period, from three in a seven-day period to just one.1 Other reported outcomes included:1 32% wounds healed by the final visit 50% reduction in wound area in four weeks in 75% of patients Two thirds (68.7%) reduction in wound area from baseline to the final visit Reduced pain at dressing changes (pain severity scores of 3.1 - 3.3 at baseline associated with previously used dressings, compared to scores of 0.5 - 1.1 recorded with Mepilex® Border Flex at the final visit) 44% reduction in weekly dressing cost per patient (5.38€ less after the dressing switch) No dressing related adverse events Almost all (97%) of the clinicians rated the overall performance of Mepilex® Border Flex to be better than the previously used dressings, while 100% of patients rated Mepilex® Border Flex as ‘good’ to ‘very good’ in terms of overall satisfaction, compared to 65% for the previously used dressings. Dr Andres Roldan Valenzuela, principal investigator commented “The results of this study clearly demonstrate how simple changes to a wound care treatment regime can bring about positive outcomes for both patients and healthcare providers. At a time when healthcare systems and staff are under increasing pressure on both cost and time it is encouraging that there are solutions to help drive efficiencies and improve outcomes for all involved.” For more information, please contact: [Contact card] Sofia Lindqvist About the study design The study involved 37 adult patients, aged between 30 and 90+ years presenting with wounds that had not reduced in size by >40-50% in the previous month and had been managed with foam dressing (other than Mepilex® Border Flex), for a minimum of four weeks (baseline). Category 2 pressure ulcers (24.3%) and venous leg ulcers (18.9%) were the most common wound types. Patients in the study had Mepilex® Border Flex applied to their wounds for ≥4 weeks, in conjunction with standard of care.
-

Mölnlycke Health Care expands investment in Tamer Mölnlycke Care joint venture
The Tamer Mölnlycke Care joint venture was initiated in 2021 with the agreement to develop a customised surgical procedure tray factory in Saudi Arabia, with first production expected in Q4 2024. The increased investment allows for an expansion in the range of Mölnlycke products manufactured and distributed in the country and to the neighbouring region. Adding drapes and gowns, emollient range and selected wound care products to the offering allows more healthcare professionals and patients in the region to benefit from Mölnlycke products and solutions. Zlatko Rihter, CEO, Mölnlycke Health Care comments “To ensure we meet customer demand, geographical expansion is a strategic priority for Mölnlycke Health Care. Increased investment in our existing long-term partnership with Tamer Group will importantly enable healthcare professionals and patients in Saudi Arabia access to our quality products and solutions helping to improve outcomes, and is a step closer to realising the potential of this rapidly growing healthcare market.” Speaking on behalf of Tamer Group, Chairman Ayman Tamer adds “This investment is key to enabling future growth in the region as outlined in the Saudi Vision 2030 - supporting the regional healthcare ecosystem, including exporting goods to the Middle East and Africa region, whilst developing local skills and expertise.” Mahmoud Wagih, CEO, Tamer Mölnlycke Care comments “I am delighted to lead this business where Mölnlycke and Tamer will build a strong, long-term successful joint venture, bringing superior health care solutions to our region.” The Tamer Mölnlycke Care joint venture is a long-term agreement between two organisations who have been working in partnership over the past decade; and are committed to meeting customer demand in the evolving healthcare landscape of Saudi Arabia and the wider region. For more information, please contact: Liz Neal Director of Communications Email: liz.neal@molnlycke.com Phone: +44 7787432560
-

Mölnlycke Health Care agrees to acquire leading wound cleansing manufacturer to consolidate its position as global leader in wound care
Gothenburg 12 April 2024: Mölnlycke, a world leading MedTech company specialised in wound care and wound management, announced today it signed an agreement to acquire P.G.F. Industry Solutions GmbH, the Austrian manufacturer of Granudacyn wound cleansing and moisturising solutions. Mölnlycke and P.G.F. have worked together for five years on the manufacturing and distribution of Granudacyn, a range of solution and gel products intended for use in the cleansing, irrigation and moisturisation of various wound types. The high quality and composition of Granudacyn ensures good biocompatibility, allowing it to be effectively used on a broad range of tissues in burns, as well as acute and chronic wounds. Mölnlycke currently distributes Granudacyn in over 50 countries around the world. “With an ageing population in combination with increased chronic wounds, such as diabetic foot ulcers or venous leg ulcers, it is our obligation to help ease the burden of wounds on national healthcare regimes” says Zlatko Rihter, CEO of Mölnlycke Health Care. “The acquisition of P.G.F. and its state-of-the-art manufacturing plant, will allow Mölnlycke to aggressively expand our Granudacyn business to improve the lives of even more patients.” “I’m excited for P.G.F. to become part of Mölnlycke and for the team to continue to manufacture products that support Mölnlycke’s Wound Care mission to help free patients from the burden of wounds” says Peter Fritz, P.G.F. founder and CEO, who will continue to lead this team and manufacturing process from P.G.F.’s Austria headquarters. Closure is expected after certain milestones are reached and will be communicated separately. For more information, please contact: Jennifer Doak Global Communications Director Wound Care Email: jennifer.doak@molnlycke.com Phone: +1 678 206 6179 About Mölnlycke® Mölnlycke Health Care is a world-leading MedTech company that specialises in innovative solutions for wound care and surgical procedures. Mölnlycke products and solutions are used daily by hospitals, health care providers and patients in over 100 countries around the world. Founded in 1849, Mölnlycke is owned by Investor AB and headquartered in Sweden. www.molnlycke.com About P.G.F. Industry Solutions P.G.F. Industry Solutions was founded in 2005 by Peter Fritz to develop and produce ecologically compatible hypochlorous acid based products to protect the user and their environment. The company is founded on more than 30 years of experience in research, development, production, and worldwide distribution of medical and measurement products. P.G.F. employs approximately 25 employees and is headquartered in Elixhausen, Austria. www.veriforte.com.
-

Mölnlycke signs a EUR 350 million revolving credit facility
The facility is backed by a group of seven leading global and regional banks, well diversified to match Mölnlycke’s geographical footprint. The banks are BNP, Danske Bank, HSBC, ING, JP Morgan, Nordea and SEB as mandated lead arrangers. SEB acted as the coordinator, documentation agent and facility agent for the transaction. For more information, please contact: Liz Neal Director of Communications Email: liz.neal@molnlycke.com Phone: +44 7787432560 About Mölnlycke Mölnlycke is a world-leading medical products and solutions company that equips healthcare professionals to achieve the best patient, clinical and economic outcomes. The core business is within the four Business Areas Wound Care, Operating Room Solutions (ORS), Gloves and Antiseptics. Mölnlycke employs around 8,700 people. The headquarters are in Gothenburg, Sweden, and the company operates in more than 100 countries worldwide. Mölnlycke is owned by Patricia Industries AB, which is part of Investor AB, an engaged owner of high-quality, global companies founded by the Wallenberg family in 1916. www.molnlycke.com
-
Mölnlycke Health Care announces launch of the 2025 Future Summit
“At Mölnlycke, we believe that education is a cornerstone of progress in healthcare. The 2025 Future Summit exemplifies our commitment to fostering innovation, enhancing clinical practice, and building partnerships that enable healthcare professionals to improve patient outcomes”, says Emma Wright, Chief Medical Officer at Mölnlycke Health Care. “We are thrilled to bring together such a diverse and accomplished group of experts to shape the future of wound care.” Offering a unique platform for collaboration Set to be a highlight of the professional education calendar, the 2025 Future Summit will host over 130 HCPs from vascular, orthopedic, general, and plastic surgery specialties. With the participation of global faculty leaders, the event will provide a unique platform to explore cutting-edge advancements, share best practices, and foster interdisciplinary collaboration in wound care and surgical excellence. The summit will take place on October 6-7, 2025, in the Netherlands and will be presided over by renowned experts Professor Javad Parvizi and Mr. Ibby Younis. “The Future Summit reflects the power of partnership and education in driving medical advancements,” says Professor Javad Parvizi, co-president of the summit. “By bringing together experts from diverse specialties, this event creates a unique opportunity to exchange knowledge and redefine standards in wound care and surgery.” A catalyst for innovation Attendees of the summit will be provided with the opportunity to engage in meaningful dialogue, access the latest clinical insights, and participate in interactive workshops led by global faculty leaders. “This summit is not just an event; it is a catalyst for innovation. It empowers clinicians from across EMEA to collaborate, learn, and apply transformative approaches that will ultimately improve patient care. Mölnlycke’s unwavering commitment to education is truly commendable,” says Mr. Ibby Younis, co-president of the summit. For more information, please contact: Sofia Lindqvist Media Relations Manager Email: sofia.lindqvist@molnlycke.com Phone: +46 72 255 35 09
-

Mölnlycke Health Care wins Swedish Sustainability Tech award
Gothenburg, Sweden. 26 November 2024. The award ceremony was held on 25 November at the Nobel Prize Museum in Stockholm, Sweden where Susanne Larsson, CFO & EVP IT, Digital Enablement, GBS and Indirect Procurement and Caterina Camerani, VP Sustainability at Mölnlycke, accepted the award on behalf of the company. “Our ambition is to transform our business to become a global leader in sustainable healthcare. This award is proof that we are on the right track. We are dedicated to equipping our customers with innovative and sustainable healthcare solutions – for our customers, our employees, our communities and the planet,” says Caterina Camerani, VP Sustainability at Mölnlycke. Mölnlycke ProcedurePak® trays enhance efficiency¹ and help decarbonise healthcare by reducing waste and greenhouse gas (GHG) emissions². ProcedurePak® offers a sterile tray with all necessary components, reducing setup time in the Operating Room by up to 40%¹, and packaging waste by up to 90%² compared to procedures conducted with single-packed products. In one tray package, hospitals can simplify procurement and help ensure patient safety³. The streamlined workflow decreases manual tasks, alleviating stress and freeing up more time for healthcare professionals to focus on patient care. Digital tools like the Mölnlycke Portal and CO2 calculator together with ProcedurePak® Value Report allow hospitals to quantify reductions in waste and GHG emissions, aligning with both sustainability and operational objectives. The judging panel commented: “In recognition of outstanding contributions to sustainability and innovation, this year’s Swedish award celebrates a project that has significantly enhanced operational efficiency while reducing environmental impact. Their commitment to sustainability is further demonstrated by reducing waste, CO2 emissions and preparation time while ensuring patient safety.” For more information, please contact: [Contact card] Sofia Lindqvist About the Cagemini Nordic Sustainability Tech Award The Capgemini Nordic Sustainability Tech Award celebrates organisations across the Nordic region creating innovative technology solutions for a sustainable future. The urgency of the global climate crisis demands ground-breaking technology and IT service innovations that scale across industries. The Nordic Sustainability Tech Award celebrates the inspirational tech pioneers pushing the boundaries of sustainable IT and their role in limiting the environmental and social impact of climate change. References 1 Greiling. A multinational case study to evaluate and quantify time-saving by using custom procedure trays for operation room efficiency. (poster from 2010). 2 Assessing the carbon and waste benefits of moving to Procedure Packs at Royal Liverpool and Broadgreen University Hospitals, NHS Trust, 2011. 3 Optimisation of perioperative procedural factors to reduce the risk of surgical site infection in patients undergoing surgery: a systematic review Key findings P. Calò , F. Catena, D. Corsaro, L. Costantini, F. Falez, B. Moretti, V. Parrinello, E. Romanini, A. Spinarelli, G. Vaccaro, F. Venneri. Discov Health Systems 2, 6 (2023). https://doi.org/10.1007/s44250-023-00019-9.
-

Mölnlycke Health Care appoints Guillaume Joucla as Chief Financial Officer
Gothenburg, Sweden. 25 November 2024. Guillaume Joucla has been appointed new Chief Financial Officer (CFO) at Mölnlycke Health Care. Guillaume Joucla will take office as CFO and member of Mölnlycke’s Executive Leadership Team, as of 1 January 2025. Guillaume Joucla most recently comes from the role of VP Global Finance & Strategic Projects Operating Room Solutions at Mölnlycke. He has also led global cross-functional transformational programmes and held General Manager positions of local operations. Guillaume Joucla wealth of experience from his extensive career within Mölnlycke has equipped him with deep insights into the company’s operations and strategic direction. “We are thrilled to welcome Guillaume to our executive team,” said Zlatko Rihter, CEO of Mölnlycke. “His leadership and expertise will be instrumental in driving our financial strategy and supporting our growth initiatives going forward.” Guillaume Joucla has a distinguished career; before joining Mölnlycke in 2008 he held senior management roles at ProxiMed Services and BioSteril. He holds a Postgraduate degree in Finance & Management from IAE Aix-Marseille Graduate School of Management, and a Master's degree in applied mathematics from Aix-Marseille University. “I am excited to continue my journey at Mölnlycke Health Care and contribute to our ongoing success,” said Guillaume Joucla. “I look forward to working with the talented team to build on Mölnlycke’s strong foundation and contribute to our future as we revolutionise care for people and planet.” Guillaume will assume the new position as of 1 January 2025 and will be taking over from Susanne Larsson, who is leaving Mölnlycke to pursue an opportunity outside of the organisation. -Ends- For more information, please contact: [Contact card] Sofia Lindqvist
-

Mölnlycke Health Care and Operation Smile help to change people's lives with newly inaugurated cleft care centre in Philippines
Gothenburg, Sweden. 19 November 2024. The Cebu Comprehensive Cleft Care Center of Excellence is now officially inaugurated. This milestone is a result of the longstanding partnership between Mölnlycke and Operation Smile – a global non-profit charity organisation. The centre will bring comprehensive care to people born with a cleft lip or palette (CLP) in the region and is expected to serve 10,000 patients in the first three years of its operations. The incidence of babies born with cleft lip and cleft palate is higher in South-East Asia than in other regions globally. The new clinic will offer life-changing surgeries and comprehensive cleft care to patients in the region where access to healthcare services is difficult. “The support from Mölnlycke in establishing the centre is grounded in our commitment to ensure equitable access to healthcare for all and the vision we have for achieving sustainable healthcare. A part of this vision is making the centre self-sufficient, and that includes raising the level of knowledge of the local healthcare professionals in the areas where Mölnlycke can offer expertise”, comments Eric de Kesel, COO & EVP Sustainability, Mölnlycke. “Cleft patients continue to be stigmatised and we are delighted to be able to contribute to changing their lives and fully including them in society,” he adds. “This clinic is a milestone for us, but also for cleft care globally, as it is also a training hub. In a rather lengthy construction project, our partner Mölnlycke has supported us financially while, in parallel with the construction, we have jointly created and rolled out a training programme with innovative methods and solutions,” says Emiliano Romano, Executive Director, Operation Smile Philippines. “Together with some of our volunteers, clinical specialists from Mölnlycke are training the local healthcare professionals in areas such as infection prevention.” The Cebu Comprehensive Cleft Care Center of Excellence is located at the Cebu City Medical Center (CCMC) hospital, in the Philippines. It is a 2,000 m2 state-of-the-art facility providing an optimal environment for delivering comprehensive CLP services, including speech therapy, dental and psychosocial care - in addition to the areas supporting the surgical flow, in alignment with the vision of surgical care that Mölnlycke and Operation Smile share. It is also fully manned by the local healthcare workers. -Ends- For more information, please contact: [Contact card] Sofia Lindqvist About Operation Smile Operation Smile is a leading global nonprofit bridging the gap in access to essential surgeries and health care, starting with cleft surgery and comprehensive care. We provide medical expertise, training, mentorship, research and care through our dedicated staff and volunteers around the world, working alongside local governments, nonprofits, and health systems, and supported by our generous donors and corporate partners. Visit Operation Smile for more information.
Upcoming events
See all eventsKnowledge
See all articles-

Gloves | 2 min read Culture of OR safety: Double gloving for effective hand protection
Improving surgical gloving practice is about embracing a culture of safety and leading the OR team to the most effective hand protection.1 Communication is critical Preventive measures to reduce the risk of SSI, such as clean theatres, laminar air flow, good draping and skin prep, and so on, are protocol driven but rely very much on open communication policies in the OR and the surgeon setting that tone for the entire team. [Text & Image section] Nathal Communication into practice Ensuring safe OR practice also demands that gloves are donned properly, including double gloving and using a correct donning technique. The senior surgeon is responsible for staff, and should set the standard of practice for everyone in the OR. Reality: Glove barrier breaches Glove barrier breaches happen in the OR whether the injured party realises it or not. Sometimes only when removing surgical gloves does the wearer find that the gloves have been compromised. Double gloving helps protect the sterile inner glove – and hand – from bacterial contamination and keeps patient and OR staff safer, especially when an indicator glove system shows when the outer glove is breached.1 Reality: Tackling tactile sensitivity The surgical glove can affect the tactile sensitivity required, and, for Mr Coombs double gloving with high-quality surgical gloves in breast cancer surgery meant his tactile sensitivity was not affected compared to when single gloving when gripping and working with breast tissue. For surgeons, their hands are everything. Double gloving offers an efficient, cost-effective way to add that extra layer of protection during surgical interventions.2, 3 Contact us to find out more Visit Clinical Learning Hub
-

Gloves | 1 min read The new generation of (NRL) surgical gloves
Different materials like natural rubber latex used in manufacturing of medical and surgical gloves have had unintended consequences – but should NRL be reconsidered? Materials like natural rubber latex (NRL) have been a lightning rod for their impact on individuals with latex allergies. But knowing what we know now about NRL, is it time for a re-appraisal? What does the future of glove manufacture look like, and can – and should – NRL make a comeback? [Text and image section] Haydn
-

Surgical | 1 min read 10% more surgeries performed in Belgium
[video section] case berlin Dr Maurice Mommaerts, Maxillofacial Surgeon AZ Sint-Jan Bruges-Ostend hospital It has increased its number of interventions by 10% each year. The staff save time. They also comment on a more pleasant work environment and better patient care. AZ Sint-Jan Bruges-Ostend Av Maxillofacial Surgeon Dr Maurice Mommaerts said: ‘Mölnlycke Procedure trays contribute to a pleasant work environment, less stress and better use of time – in one word, efficiency.’ Director General Dr Hans Rigauts said: ‘Both nurses and doctors who use Mölnlycke Procedure Trays are clearly satisfied with them.’ [Download] case
-

Surgical | 1 min read Tray changes increase procedures by 17% in Finland
[Video section] Finland case Tarmo Martikainen, CEO at Coxa Hospital, Finland Coxa increased the number of procedures performed by 17 percent and incorporated lean processes into its daily work. [download] reference
-

Gloves | 1 min read OR sustainability: A holistic system understanding
For healthcare companies to improve their environmental impact, one step would be understanding how single-use products such as surgical gloves, influence that environmental impact. [Text & Image block] Toby Speaking the same language Whether it’s a lifecycle assessment (LCA) or disclosure standards, sustainability is only understandable and achievable if everyone within the value chain aligns on measuring and sharing data and metrics in the same way. Holistic system understanding Rather than dealing with isolated data points, it’s critical to understand an entire system. A holistic approach to improvement will consider production methods, renewability and recyclability of materials, the energy expended during production, the carbon footprint of transport, packaging, and product end of life. There’s a long sustainability journey ahead to accurately measure and understand the holistic environmental impact of healthcare delivery. Get in touch to find out more Visit Clinical Learning Hub
-

Wound care | 5 min read Rethinking surgical incision care
Surgical incision wounds, often perceived as routine and straightforward aspects of postoperative recovery, have often been overlooked and underemphasised in wound care management. This oversight can lead to suboptimal healing outcomes and increased patient suffering as well as higher costs of care. Recent insights underscore the necessity of re-evaluating incision care and the pivotal role of dressing selection in promoting effective healing. Surgical incisions: The forgotten wound? Within wound care, chronic wounds take most of the focus; they are complex and have prolonged healing processes. As a result, surgical incision wounds, which are acute by definition, may not receive as much attention from a clinical perspective. This disparity arises from the assumption that surgical wounds, being clean and surgically controlled, will heal without as much care or intervention. However, ignoring careful incision care also poses risks, such as complications like surgical site infections (SSIs) and wound dehiscence. Rethinking surgical incision care Rethinking surgical incision care advocates for a paradigm shift in how surgical incision wounds are managed. Central to this shift is the concept of undisturbed wound healing (UWH), which emphasises minimising interference with the wound site to foster optimal healing conditions. This approach involves selecting appropriate dressings that can remain in place for extended periods, thereby reducing the frequency of dressing changes and the associated risks of wound exposure and contamination. Supporting undisturbed healing is the need to create and maintain a moist environment for optimal wound healing, both in acute and chronic wounds. Adopting undisturbed wound healing as a concept means allowing the healing process to progress uninterrupted, not disturbing the wound unless absolutely and clinically necessary2, 3. It is based on maintaining a constant temperature, an optimal moist environment and keeping the wound free of external agents to facilitate the normal wound healing process. How, though, with traditional wound care protocols and conventional dressings, can healthcare providers reach an ideal undisturbed wound healing state? The critical role of dressing selection in promoting UWH Post-op incision care immediately after surgical procedure is critical. Consensus in the literature2 indicate that dressings applied in the operating theatre should remain in place for as long as possible, changed when it is clinically needed rather than based on habits or protocols. Being able to leave a post-op dressing in place for as long as possible means that dressing selection becomes critical. The ideal dressing should maintain a moist wound environment, provide thermal insulation, protect against bacterial contamination, and manage exudate effectively. Simple gauze is insufficient because it requires frequent changes and does not have the capacity or long-wearing properties of advanced dressings. Advanced wound dressings have been shown to support the needed functions, thereby facilitating UWH. By keeping the wound environment stable and protected, these dressings can reduce the risk of SSIs and promote more efficient healing. Such dressings can stay in place for longer wear as recommended, using gentle adhesives that avoid blistering and peri-wound injuries. They are designed for good exudate management and absorption, and allow patients to shower and have a free range of motion4. Clinical evidence supporting advanced dressing use Clinical studies have demonstrated the benefits of advanced dressings in surgical wound management. For instance, a consensus document by the World Union of Wound Healing Societies (WUWHS) highlights that advanced dressings play a vital role in protecting wounds from surgical complications during the healing process. These dressings not only provide a barrier against external contaminants but also create an optimal environment for cellular activities essential for wound repair. Economic considerations and patient outcomes While advanced dressings may incur higher initial costs compared to traditional gauze, the overall economic impact works out to be a lower cost of care when considering the bigger picture. The use of advanced dressings can lead to fewer dressing changes, reduced labour costs for healthcare providers, and a decrease in the incidence of complications that require additional treatments. Moreover, improved patient outcomes, such as faster healing times and reduced discomfort, contribute to enhanced patient satisfaction and quality of life. Implementing best practices in incision care Optimising surgical incision care will require rethinking incision care, dressing protocols and dressing selection. Healthcare providers are on the frontlines and should consider the following best practices: Assessment of wound characteristics: Evaluate the wound's size, location, exudate level, and patient-specific factors to inform dressing selection. Selection of appropriate dressing: Choose dressings that support UWH by maintaining a moist environment, managing exudate, and providing a barrier to contaminants. Minimise dressing changes: Limit dressing changes to when clinically indicated, such as signs of infection or dressing saturation, to reduce disruption of the wound environment. Patient education: Inform patients about the importance of UWH, signs of potential complications, and the need to avoid unnecessary removal and change of the dressing. Monitoring and documentation: Regularly assess the wound and document its progress to ensure timely identification of any issues and to adjust care plans accordingly. Making incision care matter Surgical incision wounds should no longer be the forgotten aspect of wound care. By rethinking incision care and prioritising the selection of advanced dressings that facilitate undisturbed wound healing, healthcare providers can improve patient outcomes, reduce complications, and achieve more efficient use of healthcare resources.
-

Gloves | 1 min read Creating a Consensus document for surgical gloving best practice – Part 1
Hands are the most important tool in the operating room and gloves are protecting the hands and are an essential part of maintain the aseptic barrier during the surgical procedure. Many glove users don’t know how gloves are made and the different materials they can be made of, and what impact that might have on durability and performance. Neither are most users aware that there is a wealth of styles of surgical gloves to choose from, with different fit on the hand. At the end of the day, these differences could actually affect surgical performance and safety as well as long term hand health. [Text & Image section] Dr Todd Brindle
-

Gloves | 1 min read Creating a Consensus document for surgical gloving best practice - Part 2
In part two, Dr Brindle recognizes that different countries will have adopted their own gloving practice. The challenges to overcome as new recommendations for gloving best practice, entirely based on scientific evidence, are presented, is to make sure these are implemented with the evidence for why the change needs to happen clearly expressed. The systematic reviews talked about in this episode, will certainly clarify the need for the change to happen to ensure improve safety of the patient and the health care provider alike. [Text & Image section] Part 2 Todd Brindle
-
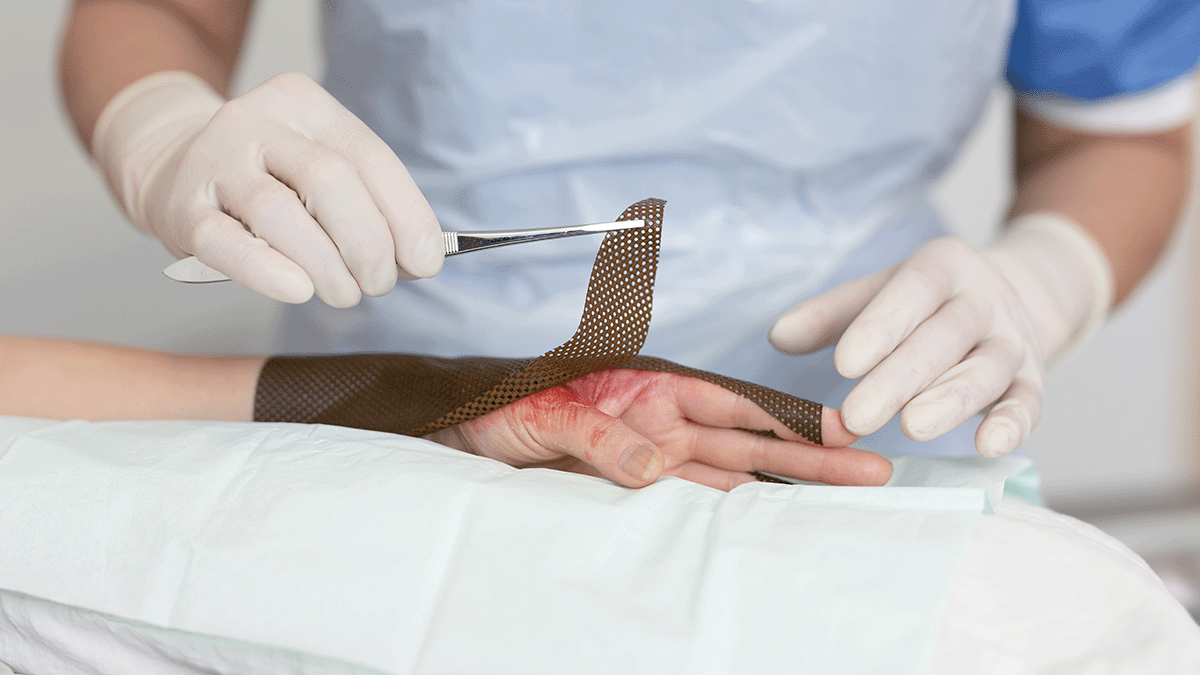
Wound care | 5 min read Cost-effectiveness of burn dressings
Providing cost-effective burn care is a multifaceted challenge that requires a comprehensive evaluation of various treatment modalities, particularly the selection of appropriate dressings. The choice of dressing not only influences the healing trajectory and can influence the overall cost of care. A thorough understanding of the cost-effectiveness of different burn dressings is essential for optimising patient outcomes while sustaining cost-effective care. Understanding burn wound management Serious burn wounds require complex and long-term management, potentially involving long hospital stays, time-intensive surgical and non-surgical treatments, pain management and rehabilitation. All of these have associated costs that result in burn care being expensive1. The mean cost of burn care in a burn centre is more than three times higher than the mean cost of burn care in a general hospital. The complexity and multidisciplinary nature of burn wounds make them particularly challenging, as they require comprehensive management to prevent complications, such as infections, delayed healing, and excessive scarring. Burn dressings are one key element of this management, helping to provide a moist wound environment, protecting the wound from external contaminants, and delivering antimicrobial agents when necessary. But not all burn dressings are created equally. How can the cost-effectiveness of a burn dressing be measured? Evaluating the cost-effectiveness of burn dressings The cost-effectiveness of burn dressings is determined by analysing both direct and indirect costs associated with their use. Direct costs address the price of the consumable products used at each dressing change. Indirect costs include factors, such as associated labour cost, the length of hospital stay, incidence of infection, the need for additional treatments or surgeries, and overall impact on the patient’s quality of life. A study published in the Journal of Burn Care & Research compared the cost-effectiveness of a silver-containing soft silicone foam dressing to silver sulfadiazine cream in patients with partial-thickness burns2. The randomised, multicenter trial found that the silicone foam dressing was more cost-effective, primarily due to reduced frequency of dressing changes and lower associated labour costs. Patients treated with the silicone foam dressing also experienced less pain and greater comfort, contributing to improved patient satisfaction and potentially faster healing times. Another prospective, randomised controlled trial3 evaluated four commonly used burn dressings in an outpatient setting. The study assessed factors, such as healing time, pain during dressing changes, and overall cost of treatment. The findings highlighted significant differences in performance and cost among the dressings, underscoring the importance of selecting dressings based on individual patient needs and specific wound characteristics to optimise both clinical outcomes and cost-efficiency. Total cost of care considerations When determining the most cost-effective dressing, it is important to adopt a holistic perspective that considers the total cost of care. This approach involves evaluating not only the unit cost of the dressing but also the broader economic implications of its use. For instance, a dressing that is more expensive per unit may prove to be more cost-effective in the long run if it leads to faster healing, fewer complications, and reduced need for additional interventions or hospitalisations. That is, some advanced dressings may have higher upfront costs, but their effectiveness in promoting healing and preventing complications can result in overall cost savings. Balancing cost and clinical outcomes Balancing cost considerations with clinical outcomes and efficacy is an increasingly common challenge in healthcare. Rising demand weighed against financial and resource constraints make cost containment a watchword throughout the healthcare sector. While cost is a critical factor, cost containment cannot be the sole consideration if short-term costs remove focus from long-term patient outcomes. From a procurement perspective, less expensive dressings selected solely as a cost-cutting measure can lead to higher costs in the long run, which runs contrary to the principles of value-based healthcare. Value-based healthcare (VBH) aims to achieve the best possible outcomes with existing resources, which requires looking at the big picture. With regard to dressings, a holistic approach to understanding dressing properties demands calculating for factors beyond just price. That is, what is the total cost of healing a wound? Other factors to consider in making such a calculation include characteristics, such as dressing wear time, which affects the frequency of dressing change. Fewer dressing changes reduces the number of dressings required and the time nurses spend changing dressings. Because the least expensive dressing is not necessarily the one that adds the most value, decisions regarding dressing selection should be individualised. In the case of burn dressings, taking into account the specific characteristics of the burn wound, patient preferences, and the clinical setting are important in balancing cost and clinical outcomes. Comprehensive burn care demands total cost of care considerations Providing cost-effective burn care is about more than surface-level, cost-per-unit calculations. Comprehensive burn care demands comprehensive evaluation of the total cost of care associated with different dressing options. By considering both direct and indirect costs, as well as the clinical effectiveness of each dressing, healthcare providers can make informed decisions that optimise patient outcomes while ensuring cost-effective solutions.



